British scientists have uncovered a critical step in preventing a potentially life-threatening virus called human T cell leukaemia virus (HTLV-1) from infecting human blood cells.
They have found that it may be possible to block viral infection of human cells by interfering with the proteins that envelope the virus.
Reporting in the November Journal of Virology, Dr David Brighty of the University of Dundee explains that HTLV-1 can cause an aggressive form of leukaemia when people become infected with the virus. His work is funded by the Leukaemia Research Fund, the Misses Barrie Charitable Trust and Tenovus Scotland.
Although the virus is extremely rare in the UK, it is believed to affect nearly 20 million people worldwide - mainly in areas such as Japan, Southern Africa, and the Caribbean. Approximately 5% of people infected with HTLV-1 go onto develop adult t-cell leukaemia (ATL), an aggressive form of blood cancer which is extremely difficult to treat with chemotherapy.
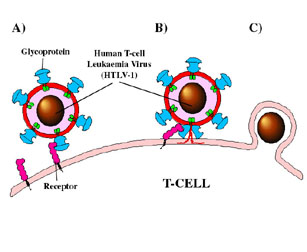
For a person to become infected, the virus must first enter a person's blood cells. This is achieved by viral proteins called envelope glycoproteins, which form spikes on the surface of the virus. These spikes enable the virus to attach to and then penetrate human blood cells known as T-cells.
When the T-cells become infected, they begin to grow and divide in an uncontrolled manner that can cause adult T-cell leukaemia. Dr Brighty has been searching for ways to stop the virus docking on the blood cells and then infecting them.
"Our studies have shown that is possible to block viral infection of blood cells by interfering with the spike proteins. It may also be possible to develop anti-viral compounds which prevent infection from taking place.
Importantly, Dr Brighty is also seeking to understand what happens once the virus has infected the T-cells. This will provide vital information about other forms of leukaemia - and other blood cancers - which also occur when T-cells grow in an uncontrolled manner.
"It is quite clear that infection with this virus is not in itself enough for a person to develop adult t-cell leukaemia. There must be a second event - or a series of genetic changes in the infected blood cells which cause these blood cells to become malignant.
"This is also believed to be the case with other forms of leukaemia - where factors such as exposure to benzene or radiation may be considered to be the first event but are not sufficient to cause the disease.
"By studying HLTV-1 infection and the events that follow we are hoping to generate a model that could provide vital information about ways of preventing other forms of leukaemia," Dr Brighty concludes.
Each year, 21,500 people in the UK are diagnosed with leukaemia, lymphoma or the related diseases.
Leukaemia Research Fund is the only national charity devoted exclusively to improving treatments, finding cures, and investigating the causes of leukaemia, lymphoma, myeloma, myelodysplasia, the myeloproliferative disorders and aplastic anaemia in children and adults.
- ends - For more information, please contact Andrew Miller on 0207 269 9019 or 07968 373406.
Notes for editors
Adult-t-cell leukaemia is hard to treat because it targets the white blood
cells that underpin the immune system. A patient with ATL has a life
expectancy of just 18 months.
Andrew Miller, Press Officer
t: 020 7269 9019
f: 020 7242 1488
e: press@lrf.org.uk
Leukaemia Research Fund, 43 Great Ormond Street, London WC1N 3JJ Registered charity 216032, a company limited by guarantee 738089